Sameer Elsayed, Western University
June 5, 2022
With cases reported in a number of countries, human monkeypox infection is generating global interest and concern as an emerging infectious disease threat even in the midst of a slowly relenting COVID-19 pandemic.
What is monkeypox virus?
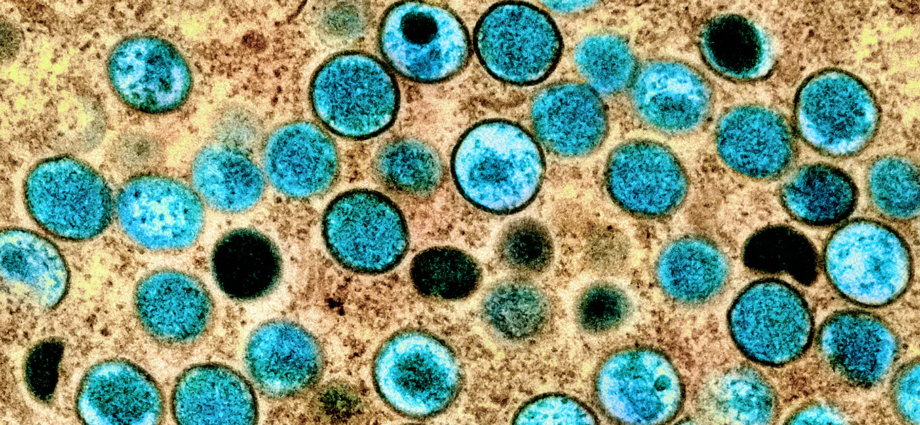
Monkeypox is a member of a closely related group of viruses in the Orthopoxvirus genus that includes smallpox, cowpox and camelpox. Monkeypox virus was first discovered in the summer of 1958 as a non-lethal, smallpox-like, skin disease of captive monkeys at a research institute in Denmark.
The name monkeypox is a misnomer since terrestrial African rodents (rats and squirrels) serve as the natural reservoir of the virus, while monkeys and other primates are believed to be accidental hosts.
When was monkeypox first reported in humans?
The first-known case of human monkeypox infection was reported from Democratic Republic of Congo in 1970, in a nine-month-old boy with a non-fatal smallpox-like illness.
Since then, sporadic human cases have occurred in many Central and West African countries, with infections being more common in children and young adults. In countries where monkeypox is endemic (where it is typically found), recent increases in cases are believed to be related to climate change, deforestation, warfare, increased population mobility and waning herd immunity from smallpox vaccination.
How is monkeypox transmitted?
Transmission occurs through close physical contact with animals or humans, their body fluids, contaminated droplet particles from respiratory secretions or infected skin lesions and indirectly by way of “fomites” (inanimate objects such as bed linens, towels and hard surfaces that may be laden with infectious virus particles).
Animal bites and consumption of animal meat are common modes of transmission in endemic areas. Secondary infections among unvaccinated close contacts occur in about 12.3 per cent household contacts and 3.3 per cent of others.
When was monkeypox first reported in non-African countries?

The first cluster of human monkeypox infections outside of Africa occurred in the United States in 2003. A multi-state outbreak involving 87 children and young adults was attributed to close contact with infected prairie dogs acquired as pets from an animal distributor. The ultimate source of infection was found to be imported Gambian rats that transmitted the infection to the prairie dogs. There were no human deaths, although three children experienced severe illness.
Prior to 2022, several travel-associated cases had been reported in the United Kingdom, Israel, Singapore and the U.S. among individuals who had visited Nigeria.
What do we know about the global monkeypox outbreak in non-endemic countries?
On May 7, 2022, public health authorities in the U.K. were informed of a case of imported human monkeypox infection in a traveller returning from Nigeria. Since then, over 550 confirmed cases of human infection have been reported in the U.K. and 29 other countries. Cases have been exceedingly higher among men who have sex with men, although the virus is not known to be sexually transmitted.
What are the symptoms of monkeypox?
The clinical manifestations of human monkeypox infection mimic those of smallpox, but are typically much milder. Unlike monkeypox, smallpox is an eradicated disease, has no animal reservoir and does not usually affect the lymph nodes.
The incubation period of monkeypox in humans ranges from four to 21 days and is followed by a one- to five-day phase of fevers, chills, sweats, fatigue and enlarged, tender lymph nodes in the neck and groin.
The next phase involves a multi-stage rash that progresses from small skin patches to papules (small bumps on the skin), followed by vesicles (small bumps filled with clear fluid) and then pustules (small bumps filled with pus). These are most prominent on the face, palms and soles of the feet. The pustules resolve by scarring or crusting over in the ensuing two to four weeks.
Exposed people may also develop a sore throat, cough and/or a rash on the mucous membranes of the mouth.
How severe is monkeypox infection?
The disease is usually mild, although severe illness and death can occur. There are two common genetic variants of monkeypox virus: the Central African variant and the West African variant. Mortality rates of 3.6 per cent for the West African variant and 10.6 per cent for the Central African variant have been reported in endemic regions.
However, no deaths have occurred to date in any of the cases reported outside of Africa. All confirmed cases from the 2022 outbreak in the 30 non-endemic countries have been due to the West African variant.
Are there any other public health recommendations for monkeypox?

People who are infected with monkeypox should wear surgical masks, and skin lesions should be covered until they have healed. Personal use items such as towels and sheets should not be shared. Frequently touched surfaces should be regularly disinfected, contaminated clothing should be laundered and contact with household and non-household members should be avoided until the illness has resolved.
Health-care workers should use gloves, gowns and respiratory protection with N95 masks and face shields, and maintain excellent hand hygiene while caring for patients with monkeypox. Hospitalized patients with confirmed or suspected monkeypox should be isolated with precautions for airborne, droplet and contact transmission until they are no longer contagious.
Does smallpox vaccine protect against monkeypox?
Smallpox vaccine — administered either before or after exposure to monkeypox — may prevent or reduce the effects of human monkeypox infection. However, rare but serious adverse events have been reported from older generation smallpox vaccines. A newer generation, non-replicating, live vaccine is now available and is deemed safe for use in all populations, including those with compromised immune systems.
The U.S. Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices recommends pre-exposure prophylaxis (vaccination prior to exposure to the virus) with the newer generation vaccine for laboratory workers performing monkeypox diagnostic testing, as well as for health-care workers administering smallpox vaccine or caring for patients with monkeypox. (Its trade name is Jynneos in the U.S., Imvamune in Canada and Imvanex in Europe.)
In Canada and other developed countries, people born before 1972 were likely vaccinated against smallpox. Although immunity following vaccination tends to wane with age, lifelong immunity appears to be the norm following smallpox vaccination in otherwise healthy individuals, and its cross-protective efficacy against monkeypox is believed to be 85 per cent.
Is monkeypox the next viral pandemic?
The emergence of infectious diseases such as monkeypox in non-endemic areas has created a great deal of anxiety in light of our experience with COVID-19.
Monkeypox had been a neglected tropical disease until the current outbreak in the developed world. But the trajectory of these cases, coupled with the pattern of transmission in Africa, suggests that the virus will not become pandemic.
The basic reproduction number (R0), a measure of viral contagiousness, where R0 equals the number of secondary infections transmitted from a single case in a non-immune population, is 0.6 to 1.0 for the Central African variant, and much lower for the West African variant.
Subscribe to our newsletter.
In contrast, the R0 for the Omicron variant of SARS-CoV-2 is approximately 10, and the R0 for measles ranges from 11 to 18. The R0 for the West African variant of monkeypox virus may be too low to sustain human-to-human transmission outside of endemic areas.
Sameer Elsayed, Professor of Medicine, Pathology & Laboratory Medicine, and Epidemiology & Biostatistics, Western University
This article is republished from The Conversation under a Creative Commons license. Read the original article.