Mansour Haeryfar, Western University
March 22, 2024
Canada is seeing a resurgence of measles, with cases in the first quarter of 2024 already far surpassing the total for all of 2023. There were 12 cases last year, and more than three times that number so far in 2024, with 38 reported as of March 19.
Most of these cases (28) are in Québec, and eight are in Ontario, while Saskatchewan and British Columbia have each reported one case.
As an immunologist with a focus on host-microbe interactions and antiviral immunity, I have been following recent measles outbreaks.
Symptoms and complications
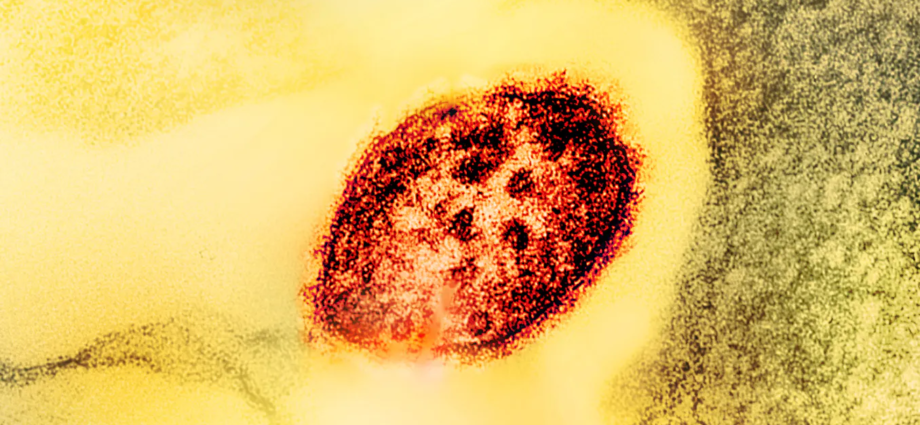
Measles (also known as rubeola) is a serious but vaccine-preventable disease caused by an RNA virus of the family Paramyxoviridae.

Measles usually begins with fever, runny nose, conjunctivitis (red watery eyes), sore throat and coughing. These can be initially mistaken for common cold or flu.
However, these non-specific signs and symptoms are typically followed by clinical manifestations that are characteristic of measles. These include Koplik spots (tiny white specks with bluish-white centres in the inner lining of the cheeks), and subsequently a measles rash appearing on the face before spreading downward to other areas of the body.
In most cases, measles resolves on its own. However, severe complications may arise, especially in immunocompromised individuals. Complications can include pneumonia, encephalitis (brain inflammation and swelling), blindness, deafness and permanent neurological consequences. When measles occurs during pregnancy, it can result in miscarriage, premature labour, stillbirth, birth defects or even fetal death. The most severe cases of measles can be fatal.
Also of note, infection with the measles virus can weaken the immune system for months or years, increasing the risk of infections with a wide range of microbes. While measles-associated immunosuppression has been documented for decades, we are only beginning to decipher its underlying mechanisms. For example, a phenomenon called “immune amnesia” is thought to contribute, at least partially, to unrelated infections in the aftermath of measles.
What is immune amnesia?
The naturally occurring (wild-type) strains of measles virus can target, infect and kill memory B and T lymphocytes, which are instrumental to antimicrobial defence. This is because one of the three measles virus receptors, called CD150, happens to be abundantly present on the surface of these lymphocytes.
Long-lived memory cells, which accumulate as a result of immunizations and infections over time, remain in a poised state to mount rapid and rigorous recall responses when we re-encounter microbes. B cells orchestrate the production of antibodies that neutralize extracellular microbes, and T cells work to destroy infected cells. Therefore, when people lose their precious memory cells to measles, the immune system is set back to a default mode, as if it has never seen any microbes or vaccines in the past.
To add insult to injury, measles virus may also eliminate “memory-like” innate T cells, which also express CD150, thus removing yet another potent weapon from our antimicrobial arsenal. Therefore, collectively, the ability of measles virus to find and kill memory and memory-like lymphocytes can lead to adaptive and innate immune amnesia, rendering a measles patient or survivor prone to many opportunistic infections.
How does measles spread and how contagious is it?

Measles virus spreads easily through airborne droplets released by infected people when they breathe, talk, laugh, cough or sneeze. In addition, measles virus infectious particles can remain active in the air and on contaminated surfaces for up to two hours.
Measles virus is one of the most contagious respiratory pathogens known, with each person with measles passing on their infection to 12 to 18 other people in a susceptible population. Measles virus is more transmissible than influenza viruses and SARS-CoV-2 variants.
How effective are measles vaccines?
Measles vaccines are safe, affordable and extremely effective. According to the World Health Organization (WHO), measles claimed 2.6 million lives each year before 1963 when a measles vaccine became available. Since then, widespread immunization programs have saved millions of lives, including an estimated 56 million just between 2000 and 2021.
Measles vaccines contain a live measles virus strain that has been attenuated so that it does not inflict harm; yet, it is sufficient to generate protective immune responses.
The measles-mumps-rubella (MMR) vaccine or the measles-mumps-rubella-varicella (MMRV) vaccine is routinely administered to children in two doses, with a first dose being given after the first birthday, typically between 12-15 months of age, followed by a booster dose recommended after 18 months of age and before attending school. This should afford lifelong protection against measles in most people.
According to the United States Centers for Disease Control and Prevention (CDC), one and two doses of the MMR vaccine are 93 per cent and 97 per cent effective in preventing measles, respectively.
Teens and adults should also remain up to date with regard to measles immunization since measles can affect anyone. There are blood tests that can be ordered by health-care providers to determine immunity to measles.
The MMR vaccine can be given at any time during one’s lifespan, but the MMRV vaccine is authorized in Canada only between one and 13 years of age.
Why are measles cases returning?
Recent years have witnessed a rise in measles outbreaks within and outside Canada. This is primarily due to an alarming decline in measles vaccination caused by delayed childhood immunizations amid COVID-19 lockdowns, vaccine hesitancy creating vulnerable societal pockets, anti-vaccine sentiments and digital misinformation spread through online social media, and the resumption of global travel post-COVID.
Measles outbreaks occur soon after herd immunity is compromised. Herd immunity is achieved when an adequately large proportion of a population becomes immune to a specific pathogen through prior infections or vaccination. As a result, the probability of an infectious case encountering a susceptible person drops dramatically.
For measles, the necessary threshold for herd immunity is 95 per cent. This means when 95 per cent of people in a population are immune, the remaining five per cent (including newborns, unvaccinated or undervaccinated children and immunodeficient people who cannot receive a measles vaccine) are also indirectly protected since the risk of measles virus transmission is significantly minimized.
By receiving two doses of a measles vaccine, one protects not only themselves but also the vulnerable members of their community. The only way to avoid measles and its serious complications, including proneness to a broad spectrum of unrelated infections, is to vaccinate widely, to engage those who are hesitant to have their children immunized in a respectful dialogue, and to educate the public regarding the unparalleled benefits of measles vaccines.
It is also crucial to isolate infected individuals for four days after the appearance of a measles rash to prevent measles virus transmission to others.
In Canada, measles has been a nationally notifiable disease since 1924 (except between 1959 and 1968), and the Canadian Measles and Rubella Surveillance System (CMRSS) ensures the weekly collection of measles data from every province and territory, including zero report submissions.
Mansour Haeryfar, Professor of Immunology, Western University
Subscribe to our newsletter.
This article is republished from The Conversation under a Creative Commons license. Read the original article.