Krista C Ritchie, Mount Saint Vincent University and Sara King, Mount Saint Vincent University
September 23, 2022
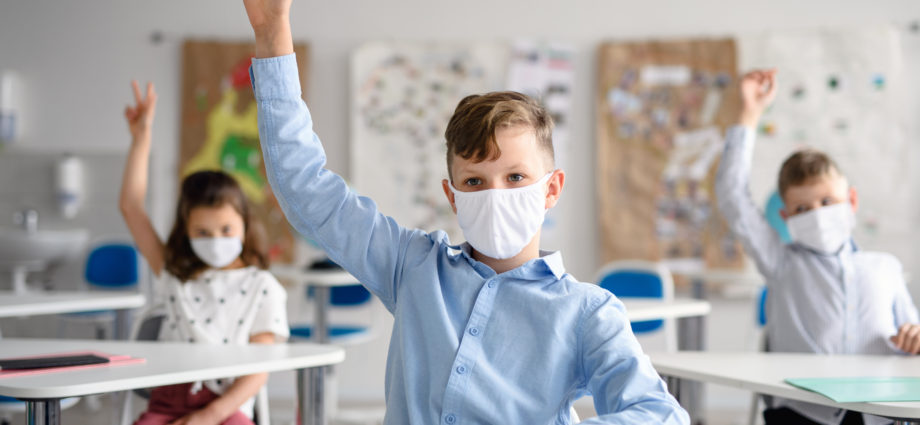
Public health pandemic responses across Canada continue to be fluid. Like other provinces, Nova Scotia has moved away from mandatory masking protocols in public spaces toward individual choice and recommendations, including in schools.
Communication to families of school-aged children directs students, teachers, and staff to make their own choice about masking.
Can a five-year-old make such a health-related decision on their own behalf? What about an 11-year-old?
From our vantage point as academics who work at intersections of education and health care, public health recommendations and provinces’ removal of clear masking requirements don’t appear to consider a child’s capacity to make decisions that affect their health.
How this “individual choice” approach plays out for students in schools needs to be carefully considered.
Who is responsible for children’s health?
As children’s rights advocates have noted throughout the pandemic, it is unethical to exclude children from conversations about issues that affect them.
However, the child’s right to be heard does not necessarily translate into being capable of making complex health-related decisions for themselves.
The World Health Organization leads global initiatives to protect the health of children and supports countries who want assistance developing their own national policies.
The federal government, in large part through Health Canada, is responsible for maintaining and improving the health of Canadians in line with the Canada Health Act.
Each provincial government is responsible for the management and delivery of health-care services.
Adult guardians hold decision-making responsibility on behalf of their children’s health.
Why, then, are students deciding for themselves whether or not to wear a mask in enclosed public spaces during a pandemic?
Ethical decision-making capacity?
For ethical reasons, fields like clinical psychology, health care and law are concerned with a person’s capacity to make decisions.
Medical researchers and doctors Craig Barstow and colleagues argue that patients have medical decision-making capacity if they can “demonstrate understanding of the situation, appreciate the consequences of their decision and reasoning in their thought process, and if they can communicate their wishes.”
The work on specifically understanding a child’s competency to make choices that affect one’s health and development is widely known in health-care and legal settings serving children and adolescents. Unfortunately, there is a paucity of research on a child’s capacity to make decisions in school settings.
Fundamentally, the criteria for being capable to make a decision are the same for children as adults.
What adults need to ask
Key questions adults need to ask themselves when determining a child’s capacity to decide include:
- What supports does the child have, and what unique risk factors might need to be considered in each context?
- Does the child understand and can they communicate the question being asked in their own words?
- Does the child have the autonomy needed to make a decision for themselves?
- Is there an established relationship with an adult whereby a child can feel comfortable asking questions to clarify understanding of the decision and potential short- and long-term consequences? Which adult is responsible for this in classrooms?
- Do guardians expect teachers to be responsible for enforcing choices parents want children to make? If so, how will teachers manage this?
- Will peer-comparison or other social pressures unduly influence the child?
- Do the responsible adults in that child’s life (guardians, teachers, school leadership, politicians establishing recommendations) understand that they are ultimately responsible for any risks that children take regarding their own health?
In Nova Scotia, unlike the legislated age to drive (16), or to vote (18), there is no specified age a child must reach before they are able to make decisions that relate to their health.
Where psychologists, social workers or physicians are involved with children’s health and wellness, the treating psychologist, social worker or physician must determine, on a case by case basis, whether a child is capable of making decisions in their best interest.
Teachers are not trained to determine capacity to decide. Have we given children a choice that they cannot make?
Difficult to assess
Decision-making capacity is difficult to assess in children, and develops from early to late childhood and into adolescence.
As explained in the psychologist Piaget’s theory of cognitive development, a child who has not yet reached adolescence is unlikely to have the capacity to think about possible futures.
This would include a child’s capacity to consider evidence in a way that helps them decide whether or not to wear a mask.
The issue for public education can be framed within one question: Who is determining students’ capacity to decide?
Adults ultimately responsible
It is critical that adults responsible for the health of children understand the complexity of decision-making capacity, so as to decide whether it is developmentally appropriate to allow students in elementary and high schools to engage in health-related decision-making.
To be clear, we are not advocating for or against any particular health recommendation or mandate. Experts in infectious diseases and public health should lead that conversation.
Subscribe to our newsletter.
However, our hope is this article raises awareness that, whereas children deserve agency in decisions that affect them, it is adults who are are ultimately responsible for fully considering the implications of federal and provincial mandates and policies on children’s rights and well-being — and subsequently for making decisions in children’s best interests.
Krista C Ritchie, Associate Professor, Faculty of Education, Mount Saint Vincent University and Sara King, Associate Professor, Faculty of Education, Mount Saint Vincent University
This article is republished from The Conversation under a Creative Commons license. Read the original article.